
They have expert knowledge of gut conditions like Crohn’s and Colitis, and can do specialist tests like endoscopies (see below). If your blood and stool tests show inflammation, you should be referred by your GP to a defined specialist gastroenterology doctor in an IBD service. Getting referred to a gastroenterology team This is because they may want to rule out more serious conditions like bowel cancer first.Īn alternative to the Faecal Calprotectin test is FIT (Faecal Immunochemical Test), which can find small amounts of blood in your stool.ģ. Your GP may also not use the Faecal Calprotectin test if you're an older adult (generally over 60 years old, but in some areas over 40). Generally, a Faecal Calprotectin result of more than 100 micrograms/g would suggest that you should have further tests for Crohn's or Colitis - although different areas use different levels.įaecal Calprotectin is not generally used to diagnose children, because the test may be less effective in people under 18. If your Faecal Calprotectin test doesn’t show inflammation in the gut, you might still have Crohn’s or Colitis – but it’s more likely that you have IBS or another non-inflammatory condition.

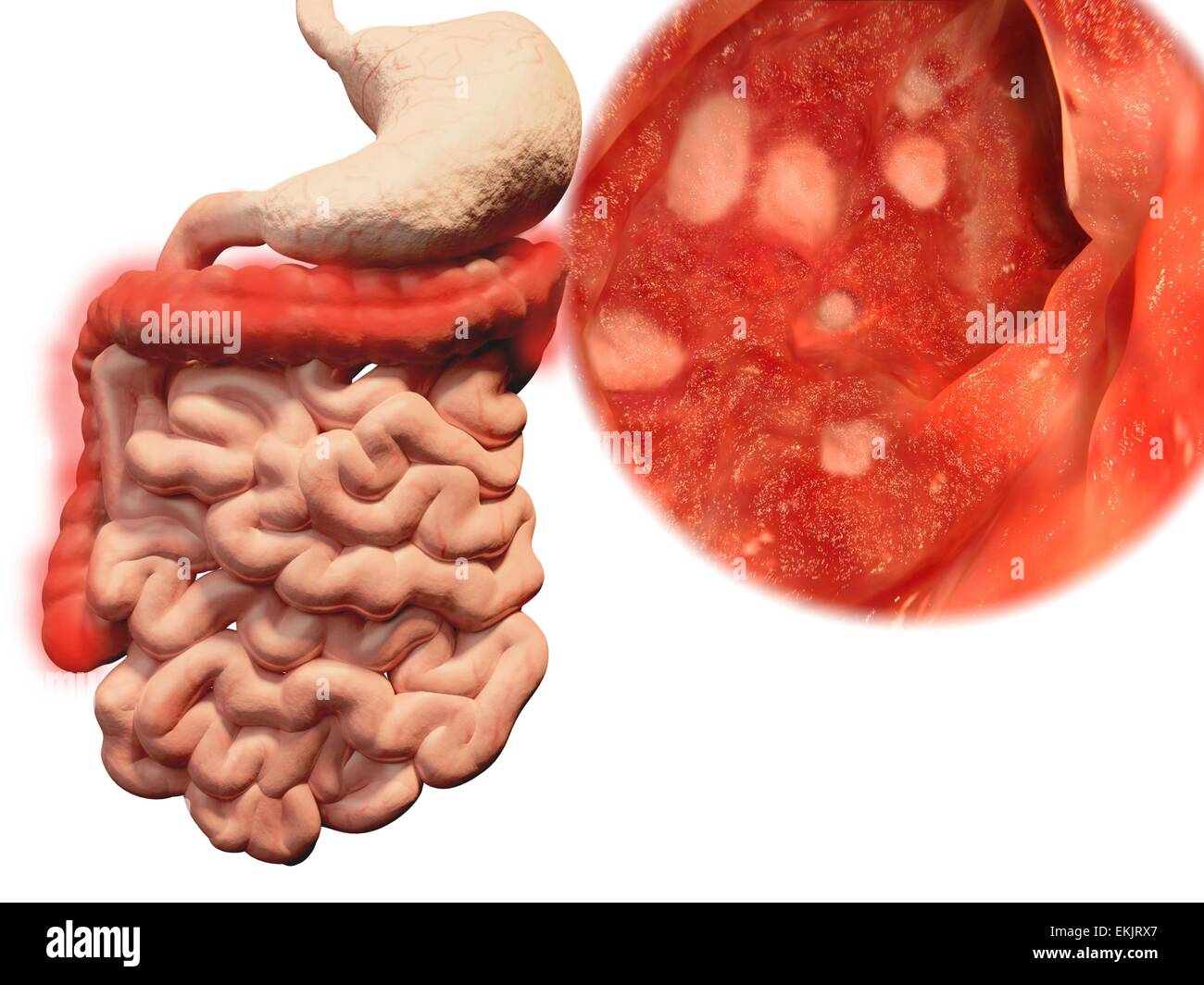
However, a high Faecal Calprotectin result can be caused by other conditions too. A Faecal Calprotectin test can show whether you have inflammation in your gut, which would be a sign that you may have Crohn’s or Colitis. It can also find signs of bleeding.Īsk your GP to test your poo for Faecal Calprotectin. Your poo can be tested to check if you have an infection that’s causing your symptoms, such as clostridium difficile (often known as c. You can take Coeliac UK's online assessment to see if you should be tested for the condition. Your GP can also order a special blood test to check for signs of Coeliac Disease. Blood testsīlood tests can show whether you have inflammation somewhere in your body and whether you are low in iron (anaemic) or other vitamins. If your GP thinks you have piles, make sure they examine you to confirm this before you're given the diagnosis. They may also check your bum (back passage) for any haemorrhoids (piles). Your GP might examine your abdomen (stomach area) to check for any lumps or tenderness. These tests can’t confirm whether or not you have Crohn’s or Colitis, but they can help narrow down the possible causes of your symptoms. The symptoms of Crohn’s and Colitis can often be quite similar to other conditions like Irritable Bowel Syndrome (IBS), so your GP should first order some tests to rule them out. You should be tested for Crohn's or Colitis if you have had abdominal pain or discomfort, bloating, or a change in bowel habit for more than 6 weeks, according to the NICE Quality Standard for IBD - though you can of course seek help sooner. See our Appointments Guide for more tips around talking to your healthcare professional, keeping track and describing your symptoms and getting the most out of your appointment.ĭon’t be afraid to ask specifically if they think it could be Crohn’s or Colitis – it could help to signpost them to the Inflammatory Bowel Disease toolkit for GPs, which has guidance for when GPs should test for the conditions.



 0 kommentar(er)
0 kommentar(er)
